Sestamibi stress test; MIBI stress test; Myocardial perfusion scintigraphy; Dobutamine stress test; Persantine stress test; Thallium stress test; Stress test - nuclear; Adenosine stress test; Regadenoson stress test; CAD - nuclear stress; Coronary artery disease - nuclear stress; Angina - nuclear stress; Chest pain - nuclear stress
Nuclear stress test is an imaging method that uses radioactive material to show how well blood flows into the heart muscle, both at rest and during activity.
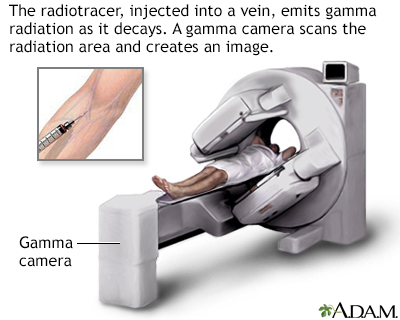
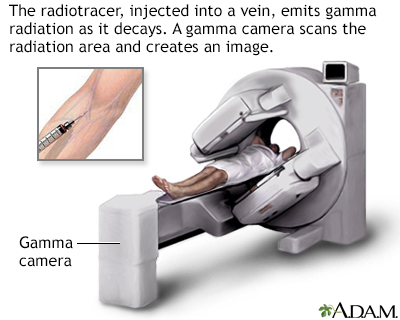
A radiotracer is injected into a peripheral vein. As the radiotracer decays, gamma radiation is emitted and is detected by a Gamma camera. When the tracer has collected in the target organ the area is scanned. Radionuclide scans can detect abnormalities such as fractures, bone infections, arthritis, rickets, and tumors that have spread, among other diseases.
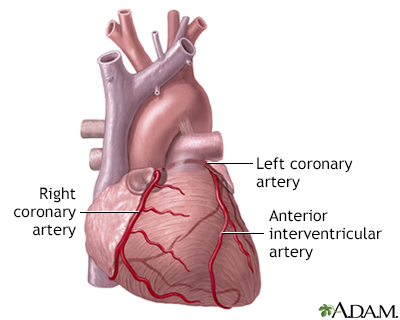
The coronary arteries supply blood to the heart muscle. The right coronary artery supplies both the left and the right heart; the left coronary artery supplies the left heart.
Your heart is the engine that keeps blood pumping throughout your body. When your heart doesn't work as well as it should, your body can't function normally. If you've had heart problems in the past, your doctor may recommend that you have a test to see how well your blood is flowing into your heart. Let's talk today about thallium and sestamibi stress test, also known as nuclear stress test. This is your heart. It's job is to receive oxygen-poor blood from your body, send it to your lungs to pick up fresh oxygen, then pump that oxygen-rich blood back out to your body. When your heart doesn't get enough blood, it can't work as well as it should. So, why would you need a thallium or sestamibi stress test? Well, your doctor may recommend that you have this test to find out why you're having chest pain, find out which treatment is best for your heart disease, check whether a treatment you've already had, such as medicine or surgery, is working, or see if you have coronary artery disease. So, what happens during the stress test? Well, you'll start to prepare for the stress test a day ahead of time. Don't eat anything the night before the test, and avoid any foods that contain caffeine for a full day beforehand. You'll have to skip your morning cup of coffee or tea, and avoid sodas and chocolate. Your doctor will let you know if you need to stop taking any of your medicines before the test. When you arrive at the doctor's office or medical center for the test, an intravenous, or IV line will be placed into your vein. Through this line, a weakly radioactive substance will be injected into one of your veins. You'll lie down and wait for 15 to 45 minutes, and a special camera will take pictures as the thallium or sestamibi substance moves into your heart during a period of rest. Then you'll walk on a treadmill with EKG electrodes monitoring your heart activity. Once you've reached your maximum level of exercise you'll get another injection of the radioactive substance and your heart will be scanned to see how well the blood is flowing during a period of stress. If you can't exercise, you'll get a drug that will simulate the effects of exercise by making your heart beat faster. During the test, some people feel chest pain, shortness of breath, dizziness, or a fast heartbeat. Let the person who is doing the test know right away if you don't feel well. So, what do the test results mean? Well, your doctor will compare the first set of images to the second set, to see if you have heart disease or your heart disease is getting worse. If blood is flowing well through the arteries of your heart, then your test is normal. If blood isn't flowing well, you may have a blockage in one or more of the coronary arteries of your heart. In that case, you may need to have another test, or an angiography, stent or heart bypass surgery to open up a blocked artery. A stress test can help your doctor see how well your heart is working. Then, you can find out together which treatments you'll need to get your blood pumping smoothly again.
Most people will then walk on a treadmill (or pedal on an exercise machine).
Your blood pressure and heart rhythm (ECG) will be monitored throughout the test.
When your heart is working as hard as it can, a radioactive substance is again injected into one of your veins.
Your provider will compare the first and second set of pictures using a computer. This can help detect if you have heart disease or if your heart disease is becoming worse.
You should wear comfortable clothes and shoes with non-skid soles. You may be asked not to eat or drink after midnight. You will be allowed to have a few sips of water if you need to take medicines.
You will need to avoid caffeine for 24 hours before the test. This includes:
Many medicines can interfere with blood test results.
During the test, some people feel:
If you are given the vasodilator drug, you may feel a sting as the medicine is injected. This is followed by a feeling of warmth. Some people also have a headache, nausea, and a feeling that their heart is racing.
If you are given medicine to make your heart beat stronger and faster (dobutamine), you may have a headache, nausea, or your heart may pound faster and more strongly.
Rarely, during the test people experience:
If any of these symptoms occur during your test, tell the person performing the test right away.
The test is done to see if your heart muscle is getting enough blood flow and oxygen when it is working hard (under stress).
Your provider may order this test to find out:
The results of a nuclear stress test can help:
A normal test most often means that you were able to exercise as long as or longer than most people of your age and sex. You also did not have symptoms or changes in blood pressure, your ECG or the images of your heart that caused concern.
A normal result means blood flow through the coronary arteries is probably normal.
The meaning of your test results depends on the reason for the test, your age, and your history of heart and other medical problems.
Abnormal results may be due to:
After the test you may need:
Complications are rare, but may include:
Your provider will explain the risks before the test.
In some cases, other organs and structures can cause false-positive results. However, special steps can be taken to avoid this problem.
You may need additional tests, such as cardiac catheterization, depending on your test results.
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;64(24):e139-e228. PMID: 25260718
Dorbala S, DiCarli MF. Nuclear cardiology. In: Libby P, Bonow RO, Mann DL, Tomaselli GF, Bhatt DL, Solomon SD, eds. Braunwald's Heart Disease: A Textbook of Cardiovascular Medicine. 12th ed. Philadelphia, PA: Elsevier; 2022:chap 18.
Fihn SD, Blankenship JC, Alexander KP, et al. 2014 ACC/AHA/AATS/PCNA/SCAI/STS focused update of the guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines, and the American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2014;64(18):1929-1949. PMID: 25077860
Flink L, Phillips L. Nuclear cardiology. In: Levine GN, ed. Cardiology Secrets. 6th ed. Philadelphia, PA: Elsevier; 2023:chap 8.
Last reviewed on: 10/5/2022
Reviewed by: Thomas S. Metkus, MD, Assistant Professor of Medicine and Surgery, Johns Hopkins University School of Medicine, Baltimore, MD. Also reviewed by David C. Dugdale, MD, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.